It’s September, which is a key month in our calendar – Childhood Cancer Awareness Month. Each year, we choose a new area to highlight because there is so much that we want people to understand about childhood cancer. This year, inspired by our recently launched Child Cancer Smart campaign, our theme is diagnosis - speeding it up and making it more accurate.
Some cancers are easier to recognise than others. People often know an unexplained lump could be a warning sign, but far fewer would realise that a new eye squint might be a symptom of a brain tumour. Brain tumours have 14 different symptoms, according to Child Cancer Smart, and can take longer to diagnose than other cancers.
On top of this, there are over 100 different types of childhood brain tumours. A child’s symptoms might suggest that a diagnosis of a brain tumour is likely – but how can doctors figure out which type it is and start the right treatment?
Could we find out more from scans?
Professor Rob Dineen at the University of Nottingham is working on a CCLG Special Named Fund research project, funded by Edie’s Butterfly Appeal, to improve ependymoma (a type of brain tumour) diagnosis.
He said: “When a child first becomes poorly with a brain tumour, they have a brain scan, usually MRI. The MRI scans are looked at by highly trained doctors (radiologists) who interpret the images to make a diagnosis of tumour type, but it can often be difficult to make an exact diagnosis due to overlaps in the scan appearances between different types of tumours.”

A child about to undergo an MRI scan.
Rob is studying how the appearance of tumours on scans relates to their underlying genetic makeup. When his project was funded in 2020, his goal was to develop a new approach to identify the types of ependymoma without the need for surgery.
He said: “Our approach has been to use a technique called ‘radiomics’, which is a computational image analysis technique that allows us to detect features in the scan images that are not visible to the naked eye. These ‘hidden’ features can then be assessed using artificial intelligence approaches that allow improvements in diagnostic accuracy.”
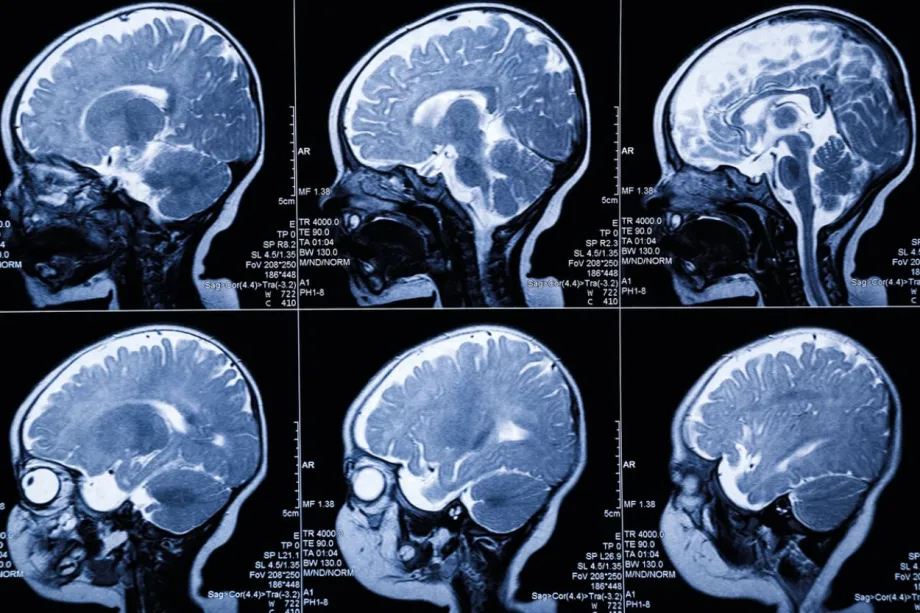
MRI scan images of a child's brain.
His team has developed a computer programme trained on MRI scans and patient data. Even with a small dataset, it has already shown it can tell apart the two main types of ependymoma (PFA and PFB), and even distinguish between two subtypes of PFA (PFA1 and PFA2). This is important because researchers think that these tumour subtypes could have different responses to treatment.
Is there something better than using an MRI for diagnosing relapses?
Professor Madhumita Dandapani began her Little Princess Trust project in 2021, aiming to develop a ‘better than an MRI’ test for ependymoma. Instead of looking at scans, she wanted to look at what tumour cells throw out.

Professor Madhumita Dandapani
In the same way that humans need to eat and get rid of waste, so do cells. Normally, the waste from cancer cells would go into the blood, but in the case of cancers like ependymoma that grow in the brain, the waste goes into the fluid around the brain. This fluid is called the cerebrospinal fluid (CSF).
Because cancer cells behave differently from normal cells, they also release different waste into the CSF than healthy brain cells. Madhumita hoped to find chemicals or proteins that, if found in the CSF, would alert doctors to even tiny amounts of living ependymoma cells.
She explained: “The aim of the research is to find a better way to detect microscopic residual tumour in children with ependymoma. Currently, half of all children with normal MRI scans at the end of treatment relapse within 2 years. This test would help us decide which patients would benefit from further treatment beyond what is currently given. This method could also be used to detect relapse or monitor response to treatment.”
By the end of Madhumita’s project in 2023, her team had analysed over 80 CSF samples from children with and without brain tumours to understand more about the chemical signatures of ependymoma in the CSF. They showed that there was a clear difference between CSF from children with ependymoma and non-brain tumour patients. This work is now being continued with funding from the Medical Research Council.
Madhumita hopes to further develop this work into a test that is “as sensitive, if not more sensitive” than a standard MRI scan. She said:
Our new testing method could help detect tiny amounts of tumour in the brain by testing the cerebrospinal fluid, even when not obviously seen on MRI scans. It could make it easier to give further treatments to these children to reduce the risk of relapse.
If successful, this kind of test could give families and doctors peace of mind much sooner and help children get the treatment they need without waiting for the cancer to show up on scans.
The future of diagnosis
Better awareness of symptoms helps families reach doctors sooner. But once children are in hospital, doctors also need sharper tools to make the right diagnosis quickly and accurately.
Projects such as these show how researchers are pushing boundaries — from teaching computers to see what humans can’t to developing tests that could one day outperform MRI scans. Each bit of research brings us closer to faster diagnoses and better outcomes for children with brain tumours.

Ellie Ellicott is CCLG’s Research Communication Executive.
She is using her lifelong fascination with science to share the world of childhood cancer research with CCLG’s fantastic supporters. You can find Ellie on X: @EllieW_CCLG