Research takes time – sometimes years or even decades. While we often see headlines about ‘breakthroughs’, real progress usually happens step by step, through many connected projects. Despite the slow progress, this is a good thing – it ensures that any changes to childhood cancer care have a solid backing of evidence.
But what if we could follow a single idea through the research journey? Well, Mr Max Pachl is a childhood cancer surgeon who has been funded by CCLG and The Little Princess Trust (LPT) for five years now, across four separate projects based at the University of Birmingham. This has enabled him to explore ways to make surgery for solid tumours, especially kidney tumours, safer…

Mr Max Pachl
2020 – 2022
Could a dye called Indocyanine Green (ICG) help?
In his first project, funded by CCLG Special Named Funds (Bethany’s Wish, Freddie’s Fight, The Georgie B Fund and Daniel’s Rainbow Fund), Max set out to discover whether a dye could make cancer surgery more effective.
“Indocyanine Green (ICG) is a well-known and safe dye,” explained Max, “which fluoresces or glows under infrared light, like how you can only see invisible ink under ultraviolet light.”
“I had heard reports that it was able to make some tumours glow when the rest of the tissues in the body did not. I thought that this might be very useful for children’s cancer surgery to show where the cancer border is and help when operating very close to important blood vessels and organs.”
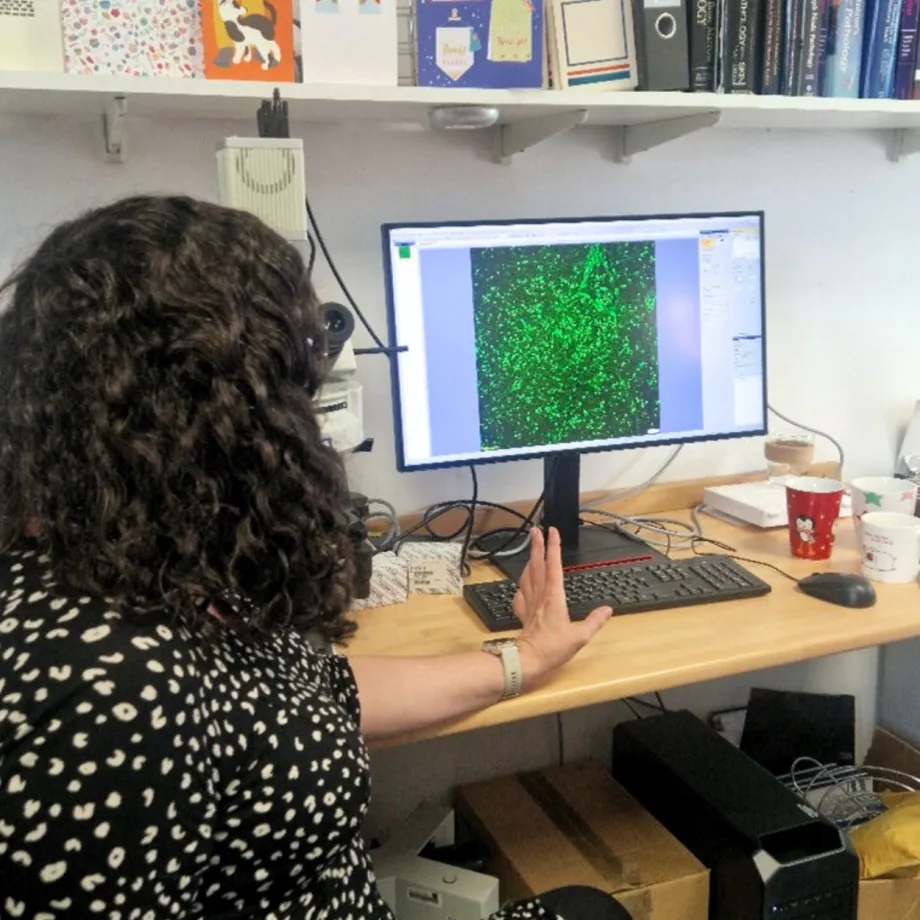
Dr Claire Bowen, a key part of Max’s team for this project, showing images of ICG dyed cells.
Through 17 childhood cancer surgeries, Max found that the dye made it easier to see the extent of the tumour being removed. The performance of the dye varied though – it was not very effective for patients who had had lots of chemotherapy, but was great for showing neuroblastoma tumours and cancer that had spread to the lungs.
The dye was also helpful for kidney cancer patients, especially for removing nearby lymph nodes. These are parts of the immune system that help fight infection but can also provide nearby cancer cells with an easy way to spread around the rest of the body.
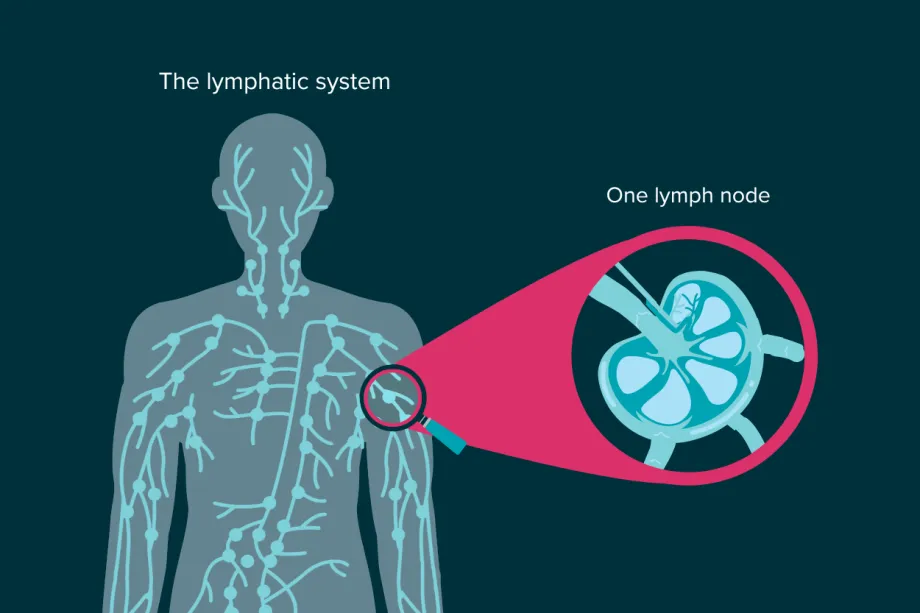
The lymphatic system is a part of the immune system. It is made up of lymph nodes and vessels, which transport white blood cells around the body to fight infection. However, cancer cells can also use this system to reach other parts of the body.
Current guidelines recommend removing lymph nodes near a kidney tumour, but they are very hard to see and are usually less than a centimetre long. ICG enabled Max to see and remove more lymph nodes, hopefully reducing the chances of the cancer growing back.
2022 – 2025
Does ICG work the same for all patients?
After these promising results, Max began working on an LPT-funded clinical trial that investigated whether the glowing ICG dye could help with multiple types of cancer surgery. The trial had a similar goal to Max’s first project, testing whether the dye could help surgeons remove more tumour and cause less damage to healthy cells, but on a much bigger scale.
The first project only looked at a small number of patients, so Max needed to look at more patients and to compare the results of ICG-guided surgery to normal surgery.
In the trial, patients are randomly assigned by a computer to either have the standard surgery to remove their cancer, or to have surgery guided by ICG. The randomisation ensures that differences in results are due to the treatment itself and not, for example, because the team chose patients with easier-to-remove tumours. Max’s project is still ongoing, but the trial is recruiting patients from multiple hospitals across the UK as well as the Princess Maxima Centre in the Netherlands, a globally recognised centre of excellence for childhood cancer.
“If the trial shows that using ICG is beneficial for a range of tumours,” said Max, “it should prompt many more centres to start using it routinely for children’s cancer – both in the UK and overseas.”
Can ICG help surgeons accurately remove kidney tumours?
After finding the ICG dye helpful for kidney cancer lymph nodes in his 2020 project, Max wanted to investigate whether ICG could further help kidney cancer patients. In 2022, he was awarded LPT funding to see whether ICG could help surgeons accurately distinguish between tumour and kidney tissue.
As a surgeon, Max is familiar with the challenges of kidney cancer surgery:
At the moment, there is no ideal way of telling where the tumour stops and the kidney starts.
"We usually find childhood kidney cancers in one kidney only, and the surgical treatment is most often to take out the tumour along with the rest of the kidney. Unfortunately, some children have cancer in both kidneys. In these children, we try to take out only the cancer and leave the normal kidney behind.”
Kidneys are vital organs with a number of important roles, including filtering waste from the blood, which is why surgeons try so hard to leave some functioning kidney tissue behind. However, this does increase the risk of leaving stray cancer cells behind, which means a higher chance of relapse and further toxic treatments for the child.
Max’s project found that ICG may help surgeons remove Wilms tumour, a type of kidney cancer: “In this study we were able to inject ICG into the kidney and tumour immediately after it had been removed to see which parts glowed and which parts did not.”
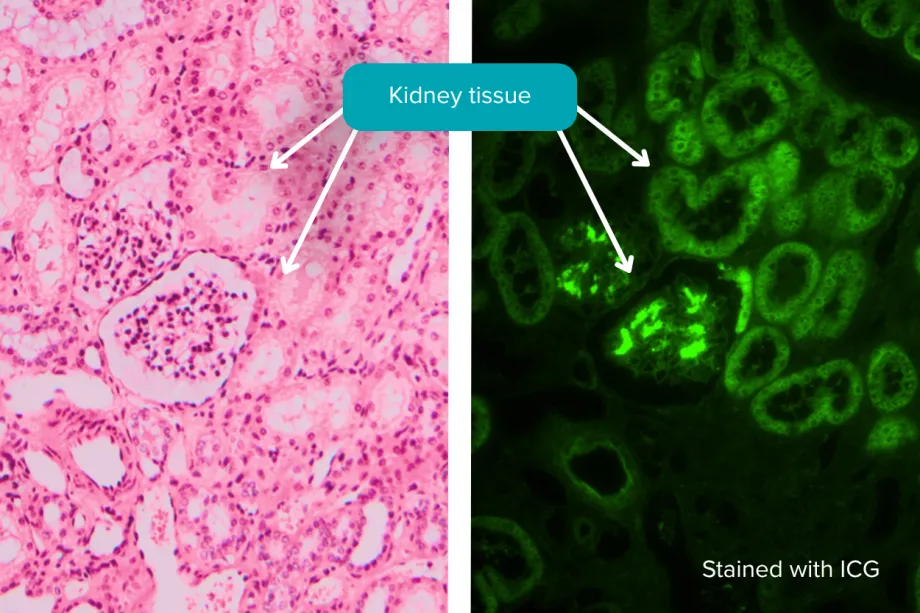
The tissue on the left is stained with standard dyes to make structures visible under the microscope, but all the tissues appear similar. With ICG staining, on the right, only the kidney tissue glows, while the blood vessels and other tissues remain dull.
After removing the tumour, Max’s team examined the edges of the glowing healthy tissue under a microscope to check if the dye had helped him take out all the cancer cells. This showed that ICG could show the difference between the healthy kidney (which glowed) and low to intermediate risk Wilms tumour cells (which didn’t). However, Max was surprised to find that high-risk tumours did take up the dye and glow – meaning that this method couldn’t be used for high-risk kidney cancer surgeries.
2024 – 2027
Is there a better way to make tumours glow?
After discovering that the ICG dye wasn’t effective for all children with kidney tumours, Max went back to the drawing board. He said:
ICG is not a perfect dye, and we still don’t understand why it works with some tumours in some patients and not in others. I wanted to have something which could show me exactly where the tumour was - not just in the kidney, but also if it had spread anywhere else in the body.
Max’s ongoing LPT-funded project hopes to provide evidence for a new fluorescent dye that can make Wilms tumour glow green. Working in the lab, Max is testing a dye called TNC, which stands for triazole N cyanine, and comparing them to ICG. TNCs are a new type of dye which glows more brightly than ICG and early research shows that it can be absorbed by cancer cells.
“TNC is a better dye in many respects,” explained Max, “as it is able to stay in the cell for longer and will probably need smaller doses. It uses the same technology and equipment as ICG, so if it works and clinical trials show it to be safe then there will be no extra requirements for new equipment.”
“My colleague at the University of Edinburgh, Professor Marc Vendrell, is an expert at working with this dye and the main bonus for me is that the dye is conjugatable.”
Conjugatable means that the researchers can attach the dye to tiny molecules that can target cancer more specifically. This means that you could create tumour specific TNC dyes or ones which only attach to cancer cells with the most aggressive genetics.
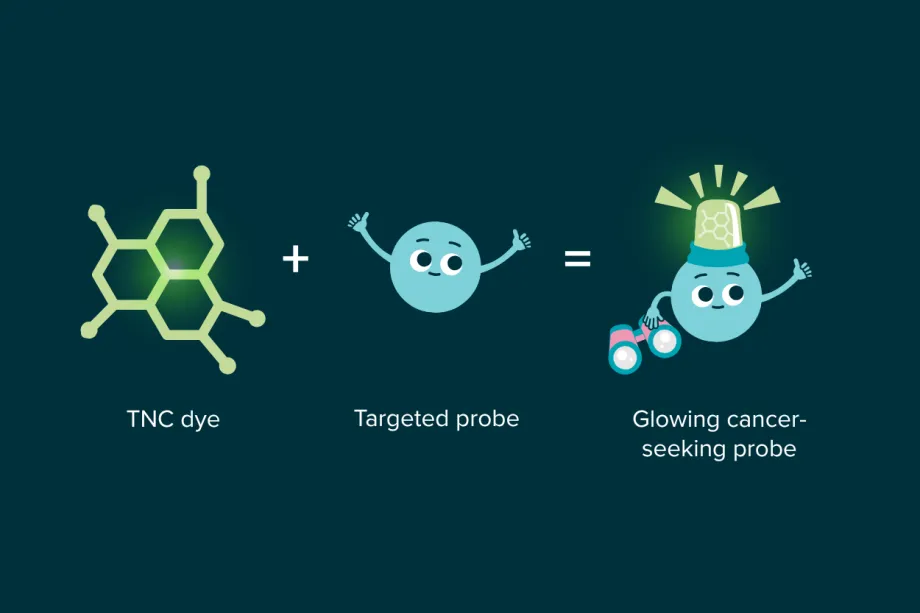
By attaching the TNC dye to a probe – something that can bind to cancer cells or their DNA – Max could create an injectable dye that would only highlight the areas surgeons need to remove.
Max is hoping to take this even further: “We know that surgery is almost the most stressful day of any patient’s cancer treatment. Making that easier, better and safer with tumour specific dyes that can also show us which bits of tumours are alive, or dead, will make targeted surgery a reality.
“If we can combine these targeted dyes with radiological imaging then this would lead to massive improvements in the overall care of our patients.”
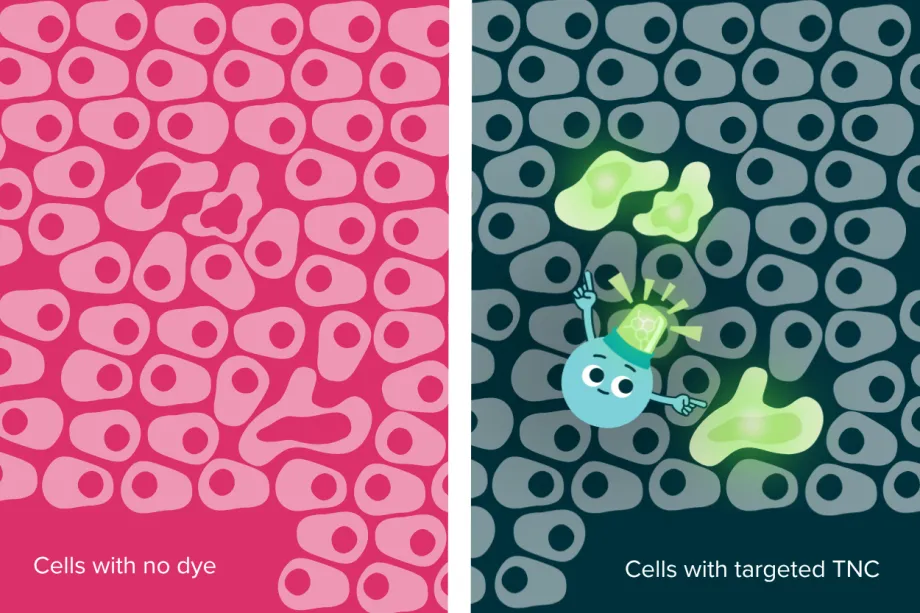
A targeted, injectable dye could highlight cancer down to the individual cell – rather than staining specific tissues.
The bigger picture
Max’s research shows how progress in childhood cancer treatment doesn’t come from one big leap, but from lots of smaller steps that build on each other. Each project has added a piece to the puzzle – testing ideas, finding what works well, and learning what doesn’t.
Outside the lab, Max volunteers with the Ellen MacArthur Cancer Trust, joining children and young people who have experienced cancer on sailing trips. There, he sees first-hand how surgery and treatment can affect every part of their lives.

Max, on the right, with Frank Fletcher, the CEO of the Ellen MacArthur Cancer Trust.
He said: “On the trips, I meet children and young people who have had cancer, and surgery, in an open and trusted environment. I can see, and we can talk about, what impact treatment has had – especially the long term physical and mental effects.”
Meeting these young people reminds Max why his research matters – and is why he won’t stop working to make surgery safer and kinder for children with cancer.

Max on one of the sailing trips with a young person who has been affected by cancer.

Ellie Ellicott is CCLG’s Research Communication Executive.
She is using her lifelong fascination with science to share the world of childhood cancer research with CCLG’s fantastic supporters. You can find Ellie on X: @EllieW_CCLG