Introduction
The tool is based on the 'A guideline to assist healthcare professionals in the assessment of children and young people who may have a bone tumour'. The guideline has been developed following careful consideration of the available evidence through a systematic review and has incorporated professional expertise via a Delphi consensus process. You can also access the full guideline, and a summary version will be produced shortly.
Click on the symptoms below to navigate individual sections of the guideline and our recommendation to either Refer/Review/Reassure.
Key symptoms
The following symptoms and signs are all associated with childhood bone tumours. Their presence should alert the clinician to this possibility.
Core symptoms
- Bone pain
- Swelling
- Bone mass/lump
- Limp/Restricted movement
Associated symptoms
- Persistent back pain especially with associated bladder/bowel/erectile dysfunction
- Fever
- Weight loss
Symptoms and signs in childhood bone tumours may occur singularly or in combination.
1. Bone pain
- Consider a bone tumour in any child with persistent* bone pain
- Ask about the presence of the other symptoms of a bone tumour (swelling, palpable lump, restricted movement/limp, fever, weight loss, back pain and bowel/bladder/erectile dysfunction) in a CYP presenting with persistent bone pain.
- Bone pain from a bone tumour can occur at any time of the day or night
- Injuries can be a red herring. Take a detailed history of the events including the onset of the symptoms after the alleged injury. Pain secondary to an injury will get better day by day.
- Bone pain can also be a symptom of leukaemia. Consider a full blood count and film in CYP where there are additional symptoms of fatigue, pallor, bruising or bleeding.
*Persistent = continuous or recurrent bone pain present on most days for 2 weeks or more
This tool works best on desktop, or by rotating your phone to horizontal
| Symptoms | Actions | |
| Reassure |
| Reassure |
| Review |
|
|
| Refer (and consider imaging) |
|
|
- Attributing symptoms to an injury incorrectly – when there is a vague or only suspected history
- Assuming that a normal X-ray findings exclude a bone tumour, especially for back or pelvic pain and when symptoms are still persisting
- Joint/limb examination: look, feel, move, assess
- Neurological examination
- pGALS examination
- Pain in spine or pelvis
- Affecting activities of daily living
- Associated neurological deficit
2. Swelling
- Swelling from a bone tumour can be discrete or diffuse
- It can occur along the long bone or around a joint
- Swelling due to a bone tumour can present with overlying erythema
- Ask about the presence of the other symptoms of a bone tumour (bone pain, palpable lump, restricted movement/limp, fever, weight loss, back pain and bowel/bladder/erectile dysfunction)
This tool works best on desktop, or by rotating your phone to horizontal
| Symptoms | Actions | |
| Reassure |
|
|
| Review |
|
|
| Refer (and consider imaging) |
*Persistent swelling present for more than 2 weeks |
|
- Attributing a red warm swelling to infection despite no improvement with antibiotics
- Determine the exact duration of the swelling and characteristics of the swelling
- Determine any preceding mechanism of injury or bite/scratch
- Ask specifically for associated symptoms and risk factors: personal history of Li Fraumeni syndrome or hereditary retinoblastoma
- Joint/limb examination: look, feel, move, assess
- Neurological examination
- pGALS examination
- Swelling that is rapidly increasing in size
3. Bone mass/lump
- A bony mass/lump which is increasing in size can be a sign of a bone tumour
- Ask and examine for the other signs and symptoms suggestive of a bone tumour (bone pain, swelling, limp/restricted movement, fever, weight loss, back pain and bladder/bowel/erectile dysfunction) in CYP with a lump/mass
This tool works best on desktop, or by rotating your phone to horizontal
| Symptoms | Actions | |
| Reassure |
| |
| Review |
|
|
| Refer (and consider imaging) |
|
|
- Attributing a bony lump/mass to infection despite no response to antibiotics
- Assuming that bony lump has been present since birth and unnoticed by parents/carers prior to presentation
- Determine the exact duration and size of the lump/mass
- Determine any preceding mechanism of injury
- Ask specifically for associated symptoms and risk factors: personal history of Li Fraumeni syndrome or hereditary retinoblastoma
- Joint/limb examination: look, feel, move, assess
- Neurological examination
- pGALS examination
- With associated neurological deficit
4. Restricted movement/limp
- A bone tumour in the pelvis or lower limb can present as a limp
- A bone tumour in the upper limb can manifest as restricted movement
- Ask about the presence of the other symptoms of a bone tumour (bone pain, palpable lump, restricted movement/limp, fever, weight loss, back pain and bowel/bladder/erectile dysfunction)
- Have a high level of concern for a CYP who is normally highly active or sporty but is no longer able to play sport due to the presenting symptom
- Follow your local limping child pathway
This tool works best on desktop, or by rotating your phone to horizontal
| Symptoms | Actions | |
| Reassure |
|
|
| Review |
|
|
| Refer (and consider imaging) |
*Persistent = present for more than 2 weeks |
|
- Failure to enquire about activities of daily living
- Determine the exact duration of the limp/ restricted movement
- Determine any preceding mechanism of injury
- Ask specifically for associated symptoms and risk factors: personal history of Li Fraumeni syndrome or hereditary retinoblastoma
- Joint/limb examination: look, feel, move, assess
- Neurological examination
- pGALS examination
- Associated neurological deficit
- Previously high-level athlete, unable to continue
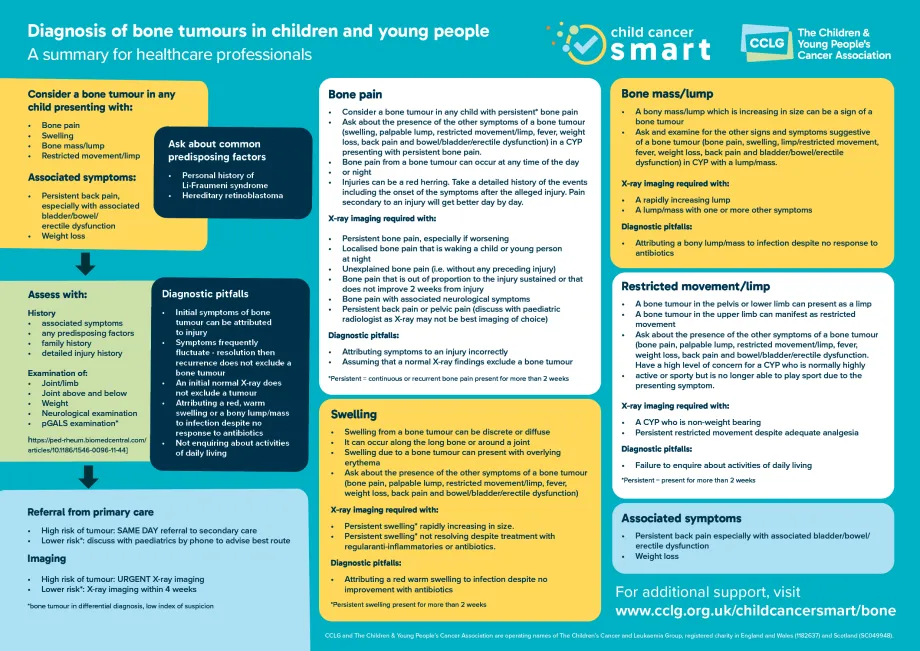
Summary poster